|
Executive Summary
|
One of the key measures for understanding the health outcomes for any country is the life expectancy at birth. As of 2016, the life expectancy in India has improved to around 66.9 years from 58.3 years in 1990.While the lower burden of communicable diseases has clearly led to higher life expectancy, social and economic evolution have led to shifting of disease patterns.
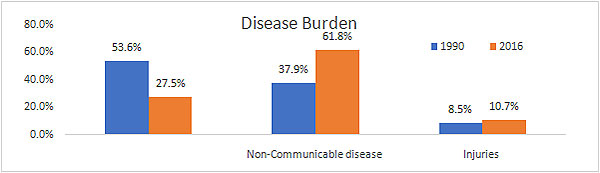
Chart 1: Shifting Disease Burden 1990 to 2016
Source: ICMR & Ministry of health and Family Welfare report 2016
Significant challenges in our healthcare infrastructure
Though deaths in India due to communicable, maternal and neonatal diseases have declined gradually, it still accounts for 16 per cent of the global share of maternal deaths and 27 per cent of global newborn deaths. Despite significant budgetary allocations over the last two decades for eradication of tuberculosis, India still accounts for 22 per cent of global incidences of tuberculosis. In addition, the incidence of non-communicable diseases continues to expand in conjunction with the rapid socio and economic developments. The public expenditure on healthcare is yet to deliver the necessary outcomes as our infrastructure does not compare well with other developing nations.
India continues to face complex challenges such as the absence of adequate infrastructure in rural and remote areas, shortage of skilled human resources, lack of standard operating practices and increasing costs.
There is a significant shortfall of around 177 per cent (till the 12th plan five year plan) in the availability of nurses. It is estimated that there is 22 per cent shortfall in primary healthcare centers and 32 per cent shortage of community healthcare centers (CHC), leading to a travel of around 100 km to access quality health care.
Access to quality care has become increasingly expensive and borne privately
It was estimated in the National Health Policy 2017 that approximately 63 million people fall into poverty each year due to lack of financial protection for their healthcare needs. The primary reason being, that around 66 per cent of the total health expenditure is borne as out of pocket expenditure (OOPE), as result of low coverage under public health scheme. Domestically, OOPE is typically funded through personal savings and borrowings and therefore it leads to high financial stress to low and middle-income groups. For comparative analysis, the OOPE for united states is 11 per cent, for China is 32 per cent and the world average is around 18 per cent.
Changing Demographics will further challenge healthcare delivery
India has a population of around 1.28 billion, with an estimated population growth rate of 1.17% and a median age of 28 years. These favorable demographics is set to witness a change over the years as we grow older as a nation. Over the next 20 years the population of our seniors would have more than doubled with an average life expectancy of 70 years and increased risk of health loss due to deteriorating lifestyle. The changing health status of the elderly make healthcare delivery a challenge.
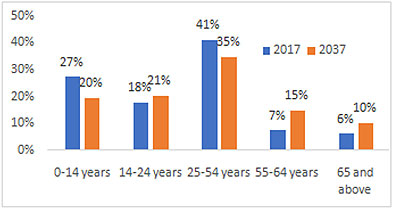 Chart 4: Population distribution for 2017 and 2037
Chart 4: Population distribution for 2017 and 2037
Source: Acuité estimates; National Health Profile 2017
A mature health care system therefore needs to include availability of adequate number of skilled and trained healthcare professionals in all healthcare settings and the government sponsored healthcare programs need to be aligned to ageing population.
Healthcare costs are expected to increase exponentially
Acuité's working model projects a significant increase in healthcare costs over the next 20 years. The model takes into account an average inflation rate of 5 per cent and has attempted to analyse the impact by categorizing the population into two distinct age groups.
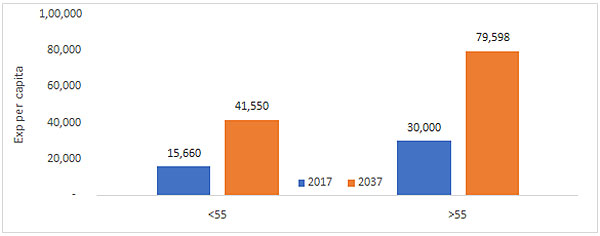 Chart 5: Increased healthcare costs amongst population groups
Chart 5: Increased healthcare costs amongst population groups
Source: Acuité estimates(All Amounts in INR).This is a single variable estimation and does not take into account budget realignments between age group, level of GDP growth and future technology improvements etc.
Excluding the impact of inflation (assumed at 5 per cent), the average per capita expenditure is estimated to increase to around Rs.19,245 per person (an overall increase of 9.7 per cent driven by an estimated 11 per cent increase in the population of elderly), which pertains only to ageing population. For the period FY18-25, if we assume the government expenditure to increase by 12 per cent to 40 per cent, the incremental burden on government is estimated to be USD 51 billion on a cumulative basis. Given such spiraling health costs, it is critical for India as a nation to adopt emerging cost-effective technologies, explore ways of making the existing infrastructure more efficient and invest in quality skilling and training programmes in healthcare.
Major part of government's current expenditure in employee salaries
Government incurs around 77-80 per cent of the expenditure towards medical and public health (salaries and expenses majorly), while the balance is somewhat equally distributed between Family Welfare and other activities (rural health is only 28% of the expenditure). The share of rural health continues to remain a small proportion of this expenditure with 70 per cent of the healthcare infrastructure in Top 20 cities of the country.
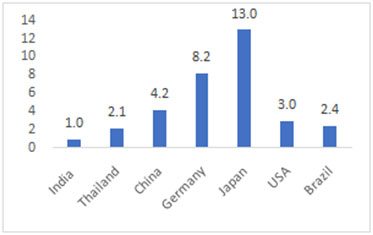
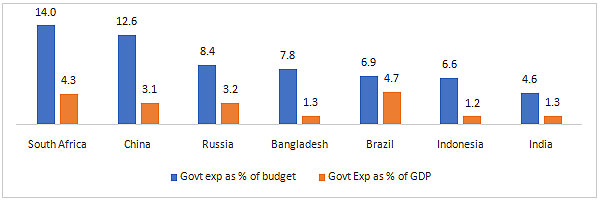 Chart 6: Per capita expenditure on health care
Chart 6: Per capita expenditure on health care
Source: WHO national health account global expenditure database
While on an absolute basis the per capita expenditure in India has increased it still remains paltry compared to other developed/developing economies.
There could be a rationale that countries richer than India are likely to have better health outcomes and better coverage, it is possible to achieve a higher return on expenditure and better outcomes through a well-structured and innovative healthcare programme.
Thailand's Universal Health Coverage Service (UCS) - A Good Example
Thailand is internationally acknowledged for achieving universal health coverage (quality health access to citizens without facing financial hardship) through its health delivery system. The success of the healthcare system in Thailand is built around policies which has ensured adequate funding, efficient delivery mechanism and availability of trained professionals.
Table 1: Key Health indicators for India in comparison to Thailand and other Upper Middle-Income nations
| Key Parameters | India* | Thailand | China | Mexico |
| GDP Per capita $ | 1712 | 5908 | 8123 | 8201 |
| Annual GDP Growth in 2016 | 7.0% | 3.2% | 7.0% | 2.3% |
| Population in 2016 (in million) | 1,280 | 69 | 1,379 | 128 |
| Health expenditure per capita in 2014 $ | 269 | 228 | 420 | 677 |
| Total health expenditure as % of GDP | 4.5% | 4.1% | 5.5% | 6.3% |
| Public health expenditure as % of total | 28.4% | 77.8% | 55.8% | 51.8% |
| OOPE as % of total health expenditure | 66.0% | 11.9% | 32.0% | 44.0% |
| Health Outcome | ||||
| Life Expectancy | 67 | 75 | 76 | 77 |
| Under 5 years mortality (per 1,000) | 55 | 12 | 11 | 13 |
| Immunizations for DPT in 2016 | 88% | 99% | 99% | 97% |
| HIV prevalence | 0.3% | 1.1% | - | 0.2% |
| Births attended by skilled staff | 38% | 100% | 99% | 96% |
*India is not an upper-middle-income country, it falls under lower middle-income
Note: World Bank considers countries of regions with a Gross National Income per capita between $3,956 and $12,235 as high middle-income economies.
Thailand made large scale investment in health infrastructure at district and sub district levels since 1990s. Health centers were continuously developed which catered to 3,000 to 5,000 people and district hospitals catered to around 50,000 to 70,000 people. In India, on the other hand, government health centers and hospitals in semi-urban and rural areas have catchment areas with population several times higher than the above.
Indian public health schemes in contrast have largely failed to achieve their objective on account of lack of infrastructure like hospital beds, doctors, diagnostic facilities etc. In addition, the quality of health outcomes, leakage of the benefits and regulations have been major contributing factors for low coverage.
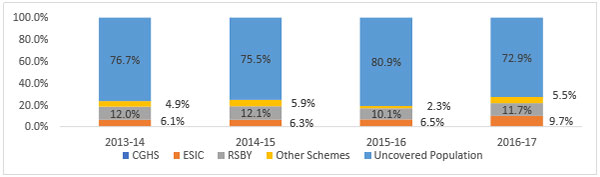 Chart 7: Uncovered Population, ministry of health and family welfare
Chart 7: Uncovered Population, ministry of health and family welfare
Source: Acuité estimates; National Health Profile 2017
Thailand's achievement is exemplary considering the demographics, which is similar to ours and therefore the learnings from this model should be implemented to achieve improvement in healthcare
Encouragingly, Government of India has launched a National Health Protection Mission (Ayushman Bharat-NHPM) in February 2018 with an initial allocation of Rs. 10,000 Cr. NHPS promises to cover about 500 million families with a sum assured of Rs. 5 lakhs. While there are concerns on the source of funding and the implementation of the scheme, it can be a potential gamechanger if adequately implemented.
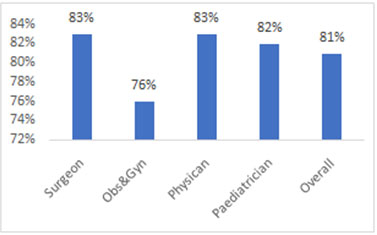
Urgent need for development of healthcare infrastructure and investment in technology
Around 70 per cent of the total healthcare infrastructure currently operational is in Tier 1 and Tier 2 cities, catering to around 27-28 per cent of the population. Currently, over 70 per cent of the ailing population and 80 per cent in rural and urban area respectively utilize private hospitals/nursing homes. Notwithstanding higher cost and lack of affordability, people prefer private healthcare facilities given the poor quality of service in state owned infrastructure.
|
Suggestions on financing healthcare infrastructure:
It is a well acknowledged fact that the taxation on tobacco/alcohol is an ever-replenishing source of fund for the government, but that alone will definitely not be able to fill in the wide funding gap.Few measures that may prove useful are enlisted below:
|
Compulsory Spending of 50 per cent of CSR on healthcare and raising minimum spend to 4 per cent of corporate profits - The company may choose to transfer the stipulated requirement with the state government and the same could be utilized for healthcare infrastructure spending. Introduction of Aushadhi Bond - Tax-saving and tax-free bonds for financing healthcare infrastructure (like NHAI bonds), which could also be open to retail investors as well through a different mechanism Pension Funds - Pension funds have a large pool of money which can be channelized through fund of funds, and the investment criteria could be redefined basis the risk assessment and government support and guarantee mechanism. Health Cess: The government may also contemplate the levy of an exclusive health cess for taxpayers in high income categories; this pool needs to be exclusively deployed for investment in specific government schemes. |